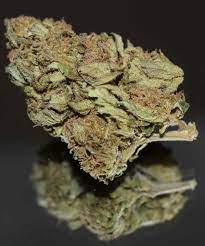
In the ever-evolving landscape of cannabis, enthusiasts and newcomers alike are often perplexed by Indica vs Sativa vs Hybrid. The spectrum ranges from the relaxing embrace of Indica to the energizing effects of Sativa, with Hybrid varieties bridging the gap. In this comprehensive exploration, we delve into the intricacies of these cannabis categories, shedding light on their characteristics and helping you navigate the vast world of weed.

Understanding the Fundamentals
Indica: Unwinding the Body and Mind
Indica strains are renowned for their calming properties, making them the go-to choice for relaxation and stress relief. Originating from the Hindu Kush mountain range, these plants are characterized by their bushy appearance and broad leaves. The cannabinoid profile of Indica strains typically boasts higher levels of CBD (cannabidiol), contributing to the soothing physical effects that ease tension and induce a serene mental state.
Sativa: Energize Your Day
On the opposite end of the spectrum, Sativa strains offer an invigorating experience, making them ideal for daytime use. Originating from equatorial regions, Sativa plants are tall and have narrow leaves. With a higher concentration of THC (tetrahydrocannabinol), the psychoactive compound, Sativa strains stimulate creativity, focus, and a sense of euphoria without the sedative effects associated with Indica.

Hybrid: Best of Both Worlds
Hybrid strains, as the name suggests, combine elements of both Indica and Sativa. Cultivators strategically crossbreed these varieties to create a diverse array of effects. Whether you seek a balance between relaxation and alertness or a tailored experience for specific activities, Hybrids offer a versatile solution. The genetic composition varies, allowing for a broad spectrum of effects to cater to individual preferences.
Indica's Embrace
Indica strains excel in promoting relaxation, making them optimal for evening use. The calming effects extend beyond the physical, soothing the mind and promoting a restful night's sleep. Popular Indica strains include Granddaddy Purple, Northern Lights, and Afghan Kush.
Sativa's Uplifting Symphony
Sativa strains are your ticket to a burst of energy and heightened creativity. Perfect for daytime adventures, these strains induce a euphoric state while maintaining mental clarity. Notable Sativa strains include Sour Diesel, Jack Herer, and Green Crack.
Hybrid Harmony
Hybrid strains offer a tailored experience, blending the characteristics of Indica and Sativa to meet diverse preferences. Whether you crave relaxation with a touch of energy or enhanced focus without the jitters, Hybrids like Blue Dream, Girl Scout Cookies, and Pineapple Express deliver a personalized journey.
Making Informed Choices
Considerations for Consumers
When selecting a cannabis strain, it's crucial to consider factors beyond the Indica-Sativa spectrum. Terpenes, aromatic compounds responsible for the distinct scents of cannabis, play a pivotal role in shaping the overall experience. Understanding the interplay between cannabinoids and terpenes empowers consumers to make informed choices based on their desired effects and flavors.

The Future of Cannabis
As legalization and research progress, the cannabis landscape continues to evolve. The future promises innovative strains, precise dosage control, and a deeper understanding of the entourage effect – the synergistic interaction between cannabinoids and terpenes. Stay tuned as the cannabis industry pioneers advancements that elevate the user experience.
